Fairport N.Y.– As the Coronavirus pandemic rages on, nursing home workers across the country are facing burnout.as they continue to battle COVID-19.
Working continuously since the beginning of the pandemic, nurses and certified nursing assistants (CNA), have been caring for the health and safety of our community’s elders- often at the risk of their own health. As long-term facilities became epicenters of the pandemic, many of these workers chose not to give up their positions, often falling ill to COVID-19 themselves as the health of their patients outweighed their own safety.
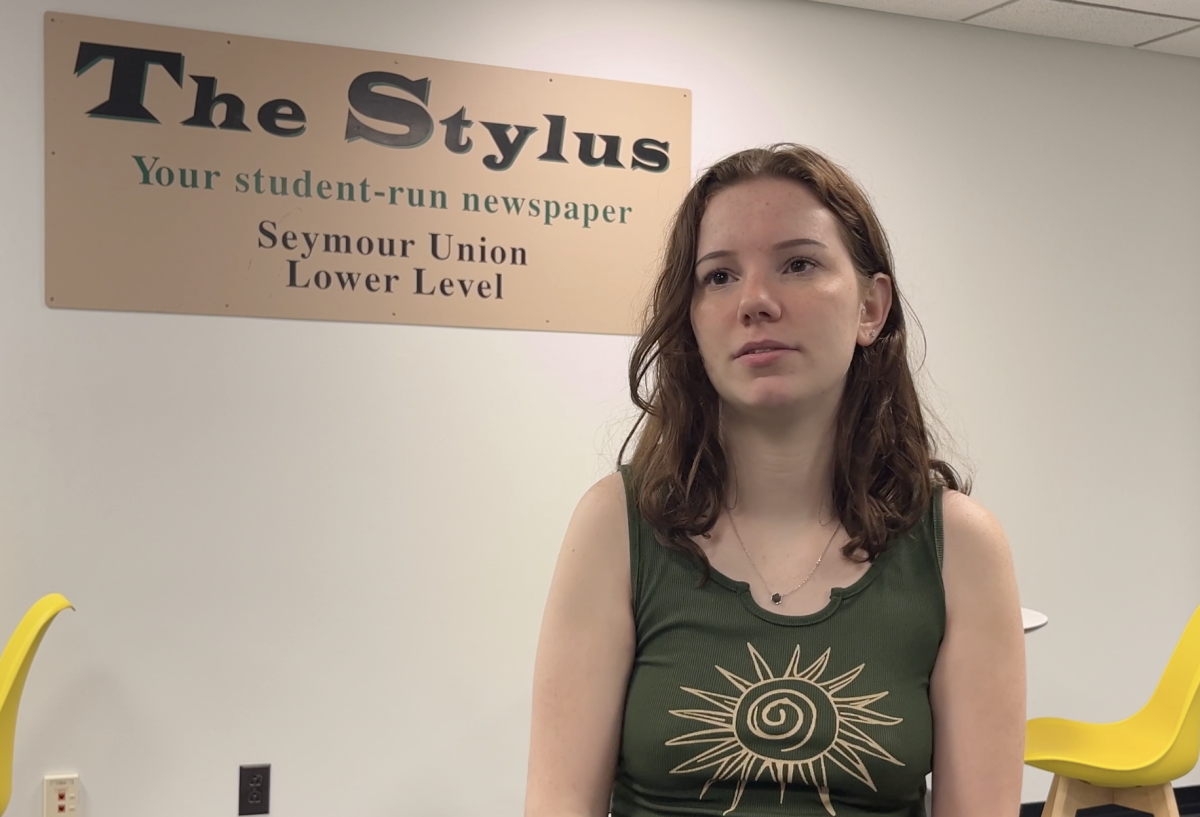
Certified nursing assistant (CNA) Emily Schutt works at Fairport Baptist Home. 22-year-old Schutt is a full-time nursing student at Nazareth University. Schutt has worked non-stop at the Fairport nursing home since the beginning of the pandemic.
“We are dangerously understaffed and as a healthcare worker I am overworking myself because of the patient to staff ratio. I feel as though if there was more media coverage on nursing homes some of these problems could be fixed,” Schutt said.
Scientific American reported that nursing home workers had one of the deadliest jobs of 2020. With visitation limited, it is difficult to know what goes on within these facilities.
“I feel as if the families of these patients don’t understand how difficult it is to work inside of these facilities,” Schutt said.
The way that nurses and aides are allowed to care for their residents has greatly changed as the pandemic progresses. CNA Janada Prior, a per diem worker at Fairport Baptist home says that the use of personal protective equipment (P.P.E) has changed patient care.
“Now we have to wear face masks and face shields at all times, and if we’re doing direct care with a resident, we have all the proper P.P.E- gowns, gloves, face mask and shield,” Prior said.
While the staff at Fairport Baptist Home did not have to face the dangers of resource scarcity, over twenty percent of nursing homes around the country did not have access to the proper personal protective equipment (P.P.E) needed for the safety of their residents and staff.
“We have to be in resident’s faces, without the proper P.P.E we put ourselves at such a greater risk of contracting COVID,” Prior said.
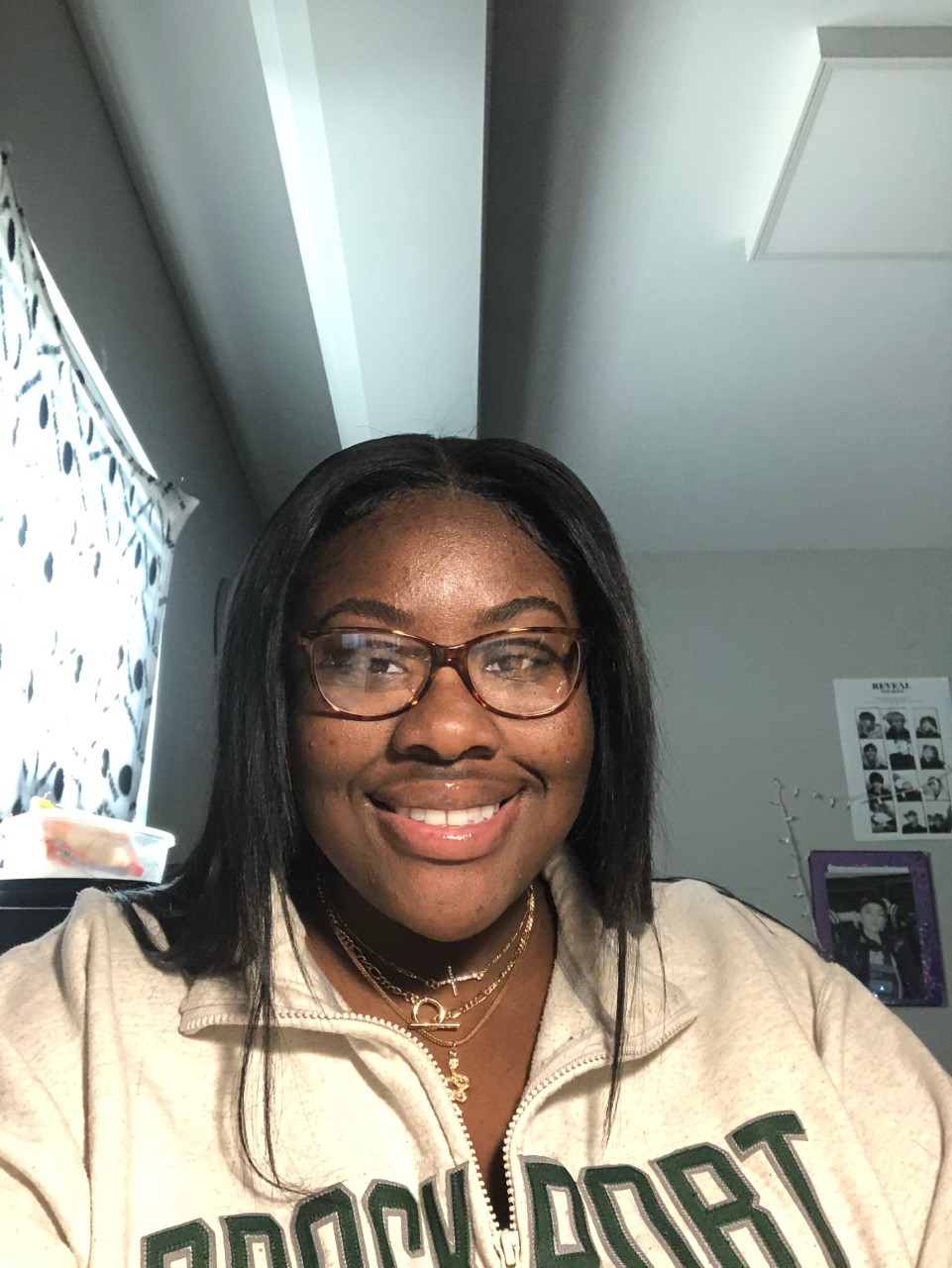
Prior, a fulltime student at SUNY Brockport, often works eight-to-sixteen-hour shifts, caring for nine to ten patients at a time. Since the beginning of the pandemic, she notes there has been a dramatic change in the way her residents act.
“We’ve had residents get so depressed that they don’t come back from it, they don’t speak, they barely eat. Some of them don’t even get dressed anymore,” Prior said.
With visitation from friends and family being halted to comply with COVID-19 guidelines, residents do not have much to look forward to, adding the stress of making sure a resident is remaining sociable to the long list of tasks staff must complete. Many residents at the home having neurological diseases, such as dementia, do not understand the reasons why their families cannot visit them.
“They just keep asking us where their families are on a loop, it takes an emotional toll, like we just feel bad for them because they’ll never know,” Prior said.
Overworked and understaffed, nursing home workers face some of the most challenging decisions everyday as they work tirelessly to provide comfort and care to older generations.